- Accreditation in Dental Practices
- Acid
- Aesthetics
- Alveolar Bone
- Amalgam
- Antibiotics
- Australian Dental Association Inc.
- Bacteria (Germs)
- Bisphonates
- Bonding
- Bridges
- Bruxism
- 3D Cone Beam [Germs]
- Caffeine
- Calculus
- Cancer
- Check ups
- Children
- Co-Planning
- Complex Reconstructions
- Composite Crowns
- Composite Resin
- Composite Veneers
- Cosmetic Dentistry
- Crowns
- Cracked Tooth
- Crown Lengthening
- Decay
- Dental Board of Australia
- Dental Board of NSW
- Dental Phobia
- Dentine
- Enamel
- Facial Proportion
- Fees
- Flexible Dentures
- Flossing
- Flouridation
- Fluoride
- Fluorosis
- Fractures
- Gingivitis
- Gold
- Golden Rule
- Guarantees
- Gum Disease Periodontitis/Periodontal Disease/Jaw Bone Disease
- Gum Surgery
- Gum/Gingiva
- Health Funds
- Immediate Implants
- Implants
- Interdental Brushes
- Invisalign
- Life On Earth
- Makeovers
- Medical Conditions and Dentistry
- Medications
- Men Only
- Mercury
- Minimally Invasive Dentistry
- Occlusal Splints/Bite Plates
- Oral Health
- Oral Hygiene
- Oral Irrigation
- Oral Pathology
- Orthodontics/Braces
- Ozone Therapy
- Parafunction
- Plaque
- Porcelain
- Porcelain Crowns
- Porcelain Veneers
- Pregnancy
- Pulp/Nerve
- Putrefaction
- Radiographs
- Registration
- Root Canal Therapy/Endodontics
- Saliva
- Sensitivity
- Shared Planning
- Sleep Apnea
- Smiles
- Smoking
- Snoring
- Soft Drinks
- Staining
- Sterilization
- Sugar
- Systemic Illness Links
- Teenagers
- Teething
- Temporo Mandibular Joint Disorder
- Tongue Cleaning
- Tooth Conditioner
- Tooth Decay
- Tooth Discolouration/Tooth Staining
- Tooth Lightening/Polishing
- Tooth Mousse
- Tooth Paste
- Tooth Sensitivity
- Tooth Whitening
- Tooth Brushing
- Toughness
- Trauma
- Valplast
- Veneers
- Vertical Dimension
- Whitening
- Women Only
- X-Rays

SYDNEY DENTAL GLOSSARY
- FAQ -
- SYDNEY DENTAL GLOSSARY
Decay
Also called "holes", caries or cavities

- Is a direct result of acids released by bacteria
- Bacteria convert sugar into acid. It is their petrol and the exhaust is the acid.
- The two best ways to avoid bacterial acid are:
- Clean your teeth properly see Oral Hygiene (Remember that bacteria multiply in minutes not months)
- Reduce sugar intake (particularly the frequency) see Diet
- Some sites collect plaque more commonly than others:
- The grooves on the biting surfaces of molar and premolar teeth especially if numerous and exaggerated (see Fissure sealants)
- The point of contact between teeth especially if food is allowed to collect there
- Along the gum/gingiva.
- And of course difficult to get at sites such as wisdom teeth
- Sometimes decay may be directly visible, others may require laser diagnosis or radiographs
- Initially, decay may appear as a small chalky area (surface demineralization called an incipient lesion) but may develop into a large cavitation. Decay may be reversed if it is only into enamel. Once it has reached dentine it cannot be reversed and should be cleaned out.
- Remember that decay can grow without causing pain [19]
- If decay is left to grow it will eventually allow bacteria into the “nerve” or pulp chamber and then tooth will require root canal therapy or extraction. Symptoms that may mean an irreversible situation requiring root therapy are:
- Stimulation of pain with heat
- Pain lasts for more than 8 minutes after removal of stimuli
- Pain without stimuli
- In severe cases, if left untreated, can lead tosepticemia; cavernous sinus thrombosis; Ludwig’s Angina and death [2,21 22 23] as did often happen in ancient times
- Rampant decay involves severe lesions on multiple surfaces of many teeth and may be seen in individuals with:
- Xerostomia or reduced saliva flow due to:
- Radiation therapy to head and neck
- Illegal stimulant drugs e.g. cocaine, marijuana, amphetamines
- c. Medications particularly neurological medications
- d. Medical conditions eg., diabetes
- Poor oral hygiene
- Large sugar intake. If rampant caries is a result of previous radiation to the head and neck, it may be described as radiation-induced caries.
- Xerostomia or reduced saliva flow due to:
- Apart from high sugar frequency, large amounts of bacteria and low saliva flow other factors which may contribute to decay include:
- Low iodine levels in saliva. Iodine is able to prevent some dental pathologies directly with antibacterial action, and also indirectly with an antioxidant mechanism.- Venturi S, Venturi M. (2009). Iodine in evolution of salivary glands and in oral health. Nutrition Health. 2009;20(2):119-34.
- Intrauterine and neonatal lead exposure promote tooth decay.[41][42][43][44][45][46][47]
- Besides lead, all atoms with electrical charge and ionic radius similar to bivalent calcium,[48] such as cadmium, mimic the calcium ion and therefore exposure may promote tooth decay. [49]
- Amelogenesis imperfecta, which occurs between 1 in 1,000 and 1 in 14,000 individuals, is a disease in which the enamel does not fully form or forms in insufficient amounts and can fall off a tooth.[26]leaving the tooth more vulnerable to decay because the enamel is not able to protect the tooth.[27]
- chewy and sticky foods (such as dried fruit and sweets) that tend to adhere to teeth longer -are best eaten as part of a meal
- Other than proper brushing and sugar reduction other factors which may prevent decay include:
- Fluoride levels before during and after tooth development
- Milk and some cheese like cheddar can help counter tooth decay if eaten soon after the consumption of foods potentially harmful to teeth.[33]
- Isolated mild casein products such as Recaldent
- Chewing gum after sugar or food,particularly if containing
- Xylitol, a sugar alcohol, cannot be used by bacteria [76]
- Use of fissure sealants
- Calcium phosphate topical creams
- With regards to epidemiology tooth decay follows the twenty eighty rule where in most countries 20% of the population accounts for 80% of decay.
Countries with least prevalence include:
- African countries
- Australia
- North America
- Scandinavian countries
- Western Europe
Countries with the greatest incidence include:
- Central and South America
- Middle East
- Eastern European nations
- India
- South East Asia
- registering dentists, students, dental specialists, dental therapists, dental hygienists, oral health therapists and dental prosthetists
- developing standards, codes and guidelines for the dental profession
- handling notifications, complaints, investigations and disciplinary hearings
- assessing overseas trained practitioners who wish to practise in Australia
- Approving accreditation standards and accredited courses of study.
- Australian Capital Territory, Tasmania and Victoria (Regional)
- Northern Territory and South Australia (Regional)
- New South Wales (State)
- Queensland(State)
- Western Australia (State)
- Registration and Notification Committee
- Immediate Action Committee
- Dentine is what the bulk of a tooth (Figs. 1 & 2) is made of and is similar in structure and composition to bone (Fig. 3)
- Dentine is less mineralised than Enamel. This together with channels or tubules (see Fig. 3) allows Decay to progress more rapidly once reached
- The Nerve inside a tooth can retreat and produce new dentine (Reparative Dentine) in response to low grade irritation such as slowly growing decay or grinding (see Fig. 4) whereas Enamel cannot be regenerated
- Fluid movement inside the tubule is responsible for tooth sensitivity. For example a blast of air over the exposed root surfaces dries out fluid at the surface which draws out fluid deeper in. This movement of fluid pulls on the nerve and registers as pain.
Acid can come from many sources: the gut; lemons; and soft drinks to name a few but the greatest damage to teeth results from bacterial waste – yes – their urine !!
Only a few specific species of bacteria are believed to cause dental caries in particular Streptococcus mutans, Lactobacilli acidophilus, Actinomyces viscosus and Nocardia spp.
Remember: Bacteria collect around the teeth and gums in a sticky, creamy-coloured mass called plaque, which serves as a biofilm
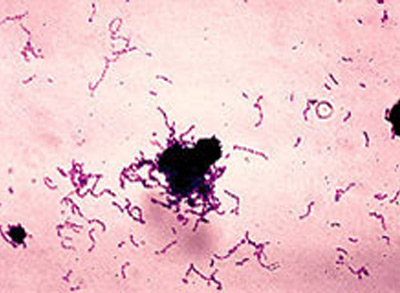
A gram stain image of Streptococcus mutans.

RHS

LHS
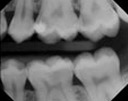
These two x-rays were taken almost exactly two years apart. This patient did not attend to fix a small hole (arrow) continued with high sugar diet and returned two years later with a painful molar requiring root canal therapy.

RHS
LHS
These two x-rays taken of the same patient on the same day show two totally different situations. The left picture is healthy with no holes whereas the right image shows numerous large lesions. This patient sat down in front of the computer at work and placed Tic Tacs only in the left cheek and the sugar from this fed bacteria throughout the day resulting in an elevated acidic environment and the holes shown at right
DENTAL BOARD OF AUSTRALIA
About the Board
Members of the inaugural Dental Board of Australia were appointed for three years by the Australian Health Workforce Ministerial Council on 31 August 2009.
Functions of the Board
The functions of the Dental Board of Australia include:
State and Regional Boards and Committees
The Dental Board of Australia is supported by State and Regional Boards which represent each State and Territory. The State and Regional Boards are as follows:
These Boards make individual registration and notification decisions, based on national policies and standards set by the Dental Board of Australia. The National Board has formally delegated the necessary powers to the State and Regional Boards.
The National Board has also appointed Committees for each State and Regional Board to deal with the registration of individuals and with notifications. These Committees have also been formally delegated powers to make certain decisions. Committees include:
Australian Health Practitioner Regulation Agency
The Board is supported by Australian Health Practitioner Regulation Agency (AHPRA) AHPRA has a National office based in Melbourne and offices in every State and Territory to support local Boards and Committees
For information about legislation governing our operations see AHPRA's Legislation & Publications.
Contact the Board
Postal address:
Dr John Lockwood, Chair
Dental Board of Australia
G.P.O. Box 9958
Melbourne VIC 3001
DENTAL BOARD OF NSW
The Dental Board of NSW deals with complaints relating to professional misconduct and infection control in the dental industry. The functions of the Dental Board are detailed in the NSW Dental Practice Act 2001. They include: protection of public health and safety, the maintenance and promotion of professional standards of dental practice in New South Wales, registration of Dentists, Dental Students, Dental Hygienists and Therapists, investigation of complaints lodged under Section 44 Dental Practice Act 2001 and administering professional conduct issues and disciplinary functions.
Contact details
Telephone number(s)
02 9281 0835
Fax number
02 9211 3606
Email(s)
information: dentalboardnsw@ozemail.com.au
Web address
http://www.dentalboard.gov.au
Office address
level 3, 28-36 Foveaux St
SURRY HILLS NSW 2010
Mailing address
PO Box K1116
HAYMARKET NSW 1240
DENTAL PHOBIA
The best way to overcome your fear is to discuss your concerns with your dentist
Experiences as a child may become distorted by time and reinforced by outdated media presentation of stereotypes. Much has changed, thanks to technology and SYDNEY DENTAL GLOSSARY Dentists are skilled professionals dealing with patients who are apprehensive about seeking treatment
This will obviously be a team approach involving you, the dentist and staff Communication is the key and for this to work you need to feel comfortable expressing your fears and concerns and have a sense that you are being listened to
At SAS Dental we are keen to change your negative thoughts into a positive experience
DENTINE

Fig. 1: Horizontal cross section of adult molar tooth showing a large band of dentine (yellow)

Figure 2: Vertical cross sections of adult canine and molar teeth showing dentine (yellow)

Fig. 3: Microscopic view of dentine showing tubules responsible for Sensitivity

Fig. 4: Wear of teeth seen in severe grinding (Bruxism). Note replacement of nerve tissue with Reparative Dentine (centre of teeth) in all but the far right tooth. Here, the tooth required Root Canal Therapy as the nerve was not able to retreat fast enough from the advancing wear
Sensitive toothpastes all work by sealing up the surface openings. Sensodyne uses potassium nitrate whereas the Colgate product “Pro Relief” uses the small amino acid Arginine see Toothpastes






